What does my coeliac disease blood test mean?
Last updated
Key Article Takeaways
- Coeliac disease is inflammation in the gut caused by an immune reaction to eating gluten.
- It’s an autoimmune disease involving antibodies.
- These antibodies also make useful blood tests for coeliac disease.
- Take our Coeliac Disease Gluten Sensitivity Blood Test to find out if you’ve got coeliac disease.
Testing for coeliac disease can be complicated, but we’re here to simplify it. We’ll discuss what is tested in a coeliac disease blood test and what your results mean.
What's tested in a coeliac disease blood test?
- Tissue transglutaminase IgA antibody (TAA) levels: this is tested in everyone. A low TAA makes coeliac disease unlikely and a high TAA means it's likely you have coeliac disease.
- Total IgA antibody level: some people have very low TAA levels and in these people we need to check their total IgA levels to make sure they're not deficient in IgA.
- Endomysial IgA antibody level (EMA): we test the EMA level in people with a high or borderline high TAA to provide confirmation of coealic disease.
- Deamidated gliadin peptide IgG antibody (DGP) level: we measure the DGP level in people who are deficient in total IgA as an alternative to the TAA test for coeliac disease.
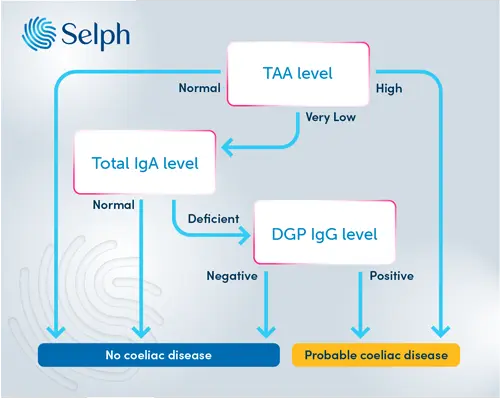
Our coeliac disease testing is based on guidance from NICE1 and follows the pathway outlined in figure 1 below. First, we test for TAA. If this is high then it’s likely you have coeliac disease. With a high or borderline high TAA level we'll also check EMA and if this is positive too then you can be almost certain you’ve got the condition.
If your TAA level is normal - not too low and not too high - then no further testing is done. You’re unlikely to have coeliac disease.
However, a “very low” TAA level suggests that you might be IgA deficient so we then check your total level of IgA antibody. If this comes back as normal (no IgA deficiency) then we don’t do any other tests. If the total IgA level is undetectable then it would suggest that you have IgA deficiency and we do the IgG coeliac disease test (DGP). A positive DGP antibody test would make coeliac disease likely.
Tell me more about antibodies in coeliac disease testing?
In coeliac disease, the body confuses gluten for something dangerous, like bacteria, which triggers an immune response. This immune response involves the body producing specific antibodies designed to attack the gluten. Unfortunately, in coeliac disease these antibodies can also target the gut lining, causing inflammation.
Antibodies are proteins in your blood produced by your white blood cells. Antibodies can stick to other cells - like bacteria - and flag them for attack by your immune system. People with coeliac disease make specific-shaped antibodies that attack certain parts of the gut lining. We can use a blood test to pick these up. In general, only people who have coeliac disease will have high levels of these antibodies so if we find them then it’s likely that you have the condition. On the other hand, if we don’t find them, then it’s unlikely you have coeliac disease.
There are a couple of antibodies we can use to test for coeliac disease. One of the most useful is an IgA type antibody that sticks to a protein in your gut called tissue transglutaminase. We call this antibody “TAA” for short.
Another antibody used in testing sticks to a protein called endomysium which makes up part of the gut lining. It’s another IgA type antibody and we call it “EMA” for short.
Lastly, there is also an IgG type antibody that’s helpful. These stick to gliadin itself and are called deamidated gliadin peptide (or DGP) antibodies.
All these antibodies (and others) have pros and cons when it comes to testing for coeliac disease but the TAA antibody probably works best and it’s the “first-line” test recommended by the National Institute for Health and Care Excellence (NICE) in the UK1.
How accurate is a coeliac disease blood test?
In general, the TAA test for coeliac disease is very accurate. If you have a positive TAA result then the chance you have coealic disease is over 90%. If you have a negative TAA result, you can be 99% sure you don't have coeliac disease2
However, some people have very low or undetectable levels (under 0.07g/L) of IgA in their blood. This is called IgA deficiency and it’s not harmful in itself. The problem is that IgA deficiency is more common in people with coeliac disease. An Italian study with 2098 participants found that 13 in 500 people with coeliac disease also had IgA deficiency, compared with fewer than 1 in 500 people without coeliac disease3. This means it's more than 10 times as likely that you’ll be IgA deficient if you have coeliac disease.
As IgA deficiency means you have little or no IgA antibody, any coeliac blood tests looking for IgA type antibodies will be negative, even if you do have coeliac disease. To overcome this, we have to use the tests for IgG type antibodies in people with IgA deficiency.
Is there anything I need to do before taking a coeliac disease blood test?
You must be eating gluten in your diet before doing a coeliac blood test. This is because antibodies against gluten are only detectable when you’re eating it in your diet. Guidelines recommend eating one or more gluten-containing meals a day in the 6 weeks before testing.
If eating gluten isn’t possible for you, a coeliac blood test won’t work. There is a genetic test which can give some information about the likelihood of your symptoms being coeliac disease, or you could see a specialist to talk about other ways to diagnose coeliac disease4.
What do my coeliac disease blood test results mean?
We’ll report your TAA levels as Normal, High, Borderline High or Very Low.
Normal
You have low levels of TAA antibodies (0.3 to 6.9 U/ml)>. This is normal for people without coeliac disease. You can be confident that you don’t have the disease. No further tests are needed. Please note that if you’ve not been eating gluten in your diet for 6 weeks prior to testing, you could get a false negative result.
High
You have high TAA antibody (≥ 10 U/ml) levels and are likely to have coeliac disease. The next step would be getting a referral to a gut specialist doctor to potentially have a camera test to check the small intestine and discuss a gluten-free diet.
Borderline High
Your TAA level is borderline high (7 - 10 U/ml). It's possible that you have coeliac disease but we can't be confident from the TAA blood test alone. We'll go on and measure your EMA level. If this is negative it's unlikely you have coeliac disease. If it's positive then it's likely you have coeliac disease.
Very Low
You have very low levels of TAA (<0.3 U/ml). We will then test your total IgA level to make sure this isn’t a sign of IgA deficiency. If the total IgA level comes back as normal, then you don’t have IgA deficiency or coeliac disease either. If you do have IgA deficiency, then we’ll check for DGP IgG antibodies. If the DGP test is negative then you don’t have coeliac disease. If it’s positive then you’re likely to have coeliac disease, so you should see a gut specialist doctor.
Get tips on better health
Sign up to our emails on the better way to better health.
We'll keep you up-to-date with the latest research, expert articles and new ways to get more years of better health.







