What you need to know about the PSA test
Published
Key takeaways on PSA testing
- Prostate cancer is the commonest cancer in men.
- A PSA test can tell you if you’re at higher risk of prostate cancer and should have further scans.
- However, a PSA test does not diagnose prostate cancer, it only tells you about your risk.
- Taking PSA tests regularly from age 45 can reduce the chance of dying from prostate cancer.
Your prostate is a walnut-sized gland sitting beneath your bladder that helps make semen. Unfortunately, it’s also the commonest site of cancer in men, with around 1-in-8 men affected during their lifetime1.
Fortunately, the PSA test you can do with one of our finger-prick collection kits at home, can help men understand their risk of having prostate cancer. But like any tool, you need to know how to use it. A screwdriver’s not much good for hammering nails but it’s still a useful tool! So let’s dive into what you need to know about the PSA test to make best use of it.
What is PSA or prostate-specific antigen?
PSA or prostate-specific antigen is a protein that’s only made in the prostate gland and helps to make semen more lubricating. Some PSA naturally leaks from the prostate into your blood where we can measure it.
PSA levels in the blood will go up as the size of the prostate increases, which happens to all men as we get older. PSA can also go up if anything “disturbs” the prostate like ejaculation, vigorous exercise or prostate cancer. In fact, the commonest way of picking up prostate cancer is because raised PSA levels in the blood gave doctors a clue it’s there.
What can cause a high PSA level?
However, lots of things can cause a raised PSA level in the blood and most of them are not prostate cancer:
- A healthy but naturally enlarged prostate (sometimes called benign prostatic hyperplasia or BPH)
- Urinary tract infection or inflammation of the prostate (prostatitis)
- Ejaculation
- Anal sex (receptive)
- Exercise (including cycling and horse riding)
- Urinary catheter insertion or a biopsy of the prostate
- Prostate cancer
What happens if I have a raised PSA level?
As we’ve said, plenty of things other than prostate cancer can cause PSA to rise so we don’t use PSA to diagnose prostate cancer. A raised PSA level only tells us that it’s more likely that someone has prostate cancer than if their PSA was normal.

If the PSA is raised, we do an MRI scan of the prostate to actually look for a cancer. Only if we see something that looks like a cancer do we go on and biopsy the prostate with a needle to actually make the diagnosis.
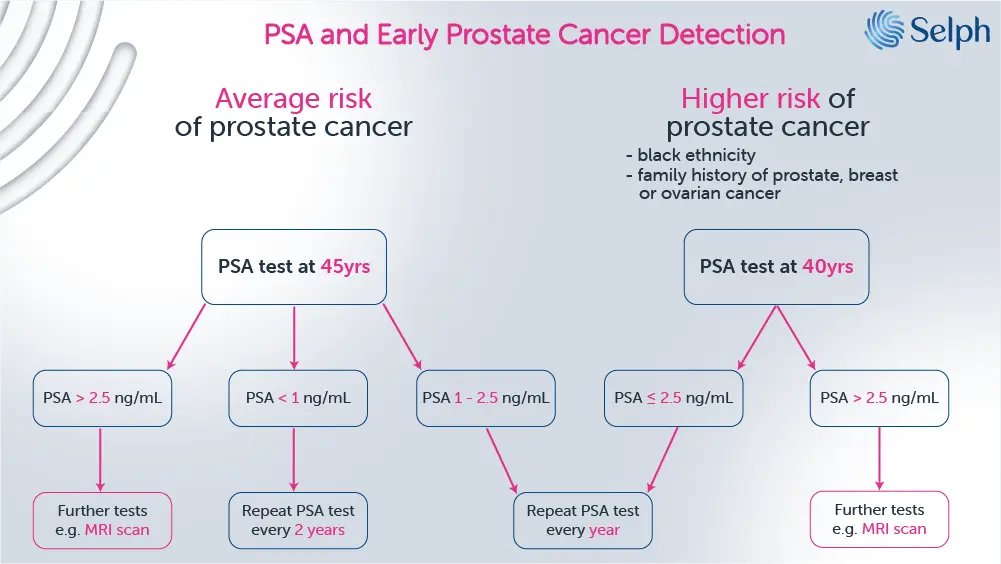
So, as you can see, the PSA test is only the first part of a pathway (figure 1 below) to diagnose prostate cancer. It just tells you about your risk of having prostate cancer. It cannot tell you if you actually have prostate cancer.

What are the benefits of taking a PSA test?
The tricky thing about prostate cancer, as well as many other cancers, is that you often won’t get any symptoms until the cancer is quite big and is more likely to have spread to other parts of the body.
Fortunately, PSA levels usually start going up well before you get any symptoms so it’s often the first clue that you might have prostate cancer. Studies show that we’re more likely to pick up prostate cancer in people who regularly check their PSA2.
Furthermore, trials have shown that men who undergo PSA screening are about 40% less likely to be diagnosed with prostate cancer that has spread2. Lastly, trials have also found that men who take a PSA test are 20-30% less likely to die from prostate cancer than men who don’t test2, 3.
Ok, so taking a PSA test has some clear benefits, but what are the downsides?
What are the downsides of taking the PSA test?
Because quite a few things can cause PSA to go up, most people (60-70%) with a raised PSA do not have prostate cancer. Naturally, many men will feel anxious while waiting for their MRI scan to see if prostate cancer is likely and this worry can last for some time even if they get the all clear.

If an MRI does suggest prostate cancer, you’d need to have a biopsy of the prostate which can be uncomfortable and carries a small risk of infection.
Although prostate cancer is common, a lot of the time it is very slow growing and will not actually cause harm or even death. It used to be quite hard to tell whether a prostate cancer was going to cause you harm and most people with prostate cancer had surgery to remove the prostate (a prostatectomy) which can cause urinary incontinence and affect erections. Put all this together and you realise that some men who were diagnosed with prostate cancer after finding a raised PSA level would never even have become aware they had the cancer if they hadn’t tested. Even worse, these men may undergo surgery with the potential for more harm than they would have experienced from the cancer itself.
Fortunately, we’re now much better at understanding who has low-risk prostate cancer and in the majority of these men, we can safely monitor the cancer and only operate if and when it poses a risk. Surgery for prostate cancer has also improved tremendously and now the standard of care is to use keyhole surgery with robotic assistance which carries a much lower risk of incontinence or erectile dysfunction.
Lastly, some men (around 15%) can have a normal PSA level but later be found to have prostate cancer. For this reason, it’s important to look at PSA levels over time rather than just a one-off level. A rising PSA level, even in the “normal” range, can still be a sign of prostate cancer.
When should I start and how often should I test my PSA?
If you’re comfortable with the risks and benefits of taking a PSA test, the next thing you need to know is when to start.
When to start depends on whether you’re at higher risk of prostate cancer than average. You’re considered higher risk if you:
- are of black ethnicity
- have a family history of prostate, breast or ovarian cancer
In the UK there is no national screening program for prostate cancer. Instead, men over the age of 50 can ask for a PSA test from their GP. However, studies have shown that having a baseline PSA test before you’re 50 can predict your risk of prostate cancer 20-30 years later4, 5. Guidelines from the USA now suggest that men begin PSA testing from age 45, or 40 if you’re at higher risk6.
Once you know your baseline PSA, you can use it to figure out how often you should check your PSA going forwards (figure 2 below).
What should I do to prepare for my PSA test?
Because anything that disturbs the prostate can raise PSA levels it’s important to avoid a few things before you to take the test:
- Avoid vigorous exercise for 48 hours before your test ( Including any cycling and horse riding).
- Avoid ejaculation or receptive anal sex for 48 hours before your test.
- Postpone your test for at least 6 weeks after a prostate biopsy, cystoscopy or urinary tract infection.
Can medications lower my PSA level?
Some medications can lower PSA levels, potentially “masking” high levels. The commonest drugs to be aware of that lower PSA are finasteride (Proscar/Propecia) and dutasteride (Avodart) which are used to treat male pattern baldness and benign prostatic hyperplasia. If you’re on one of these medications, you need to double your PSA result to estimate the “true” PSA level7.
Testosterone-lowering medications can also reduce PSA levels. But as these medications are quite specialist, it’s best to discuss PSA testing with your doctor if you take them.
The bottom line
The PSA test is one of the best tools we have to stop men dying from prostate cancer. But it’s important to understand that your PSA level tells you about your risk of having prostate cancer, not whether or not you actually have prostate cancer.
As we’ve become better at managing prostate cancer, the potential harms associated with taking a PSA test have reduced to the point where we and others, such as Prostate Cancer UK, believe the benefits outweigh the risks.
Get tips on better health
Sign up to our emails on the better way to better health.
We'll keep you up-to-date with the latest research, expert articles and new ways to get more years of better health.





